Design for
Hospital Voice Assistant (VUI)
It all started when…
In 2016, just prior to my arrival at Jefferson, an initiative to leverage smart speakers in hospital rooms was initiated with IBM. I assigned as Design Lead to the launch team to establish simple scope, clear goals, and conduct user research. In 2018 I transitioned the project with a wealth of insights and recommendations. Earlier this year Jefferson began to pilot this technology. (link to article)
Immediately upon on-boarding to this project, I worked with vendors to structure requirements and scope of early POC and conduct qualitative user research, synthesize research and create small set of skills that would lay the ground work for what would become a multi-site pilot. Prior to my participation in this project, senior stakeholders created a large list of features and nice-to-haves. Below I’ve chronicled my approach and retrospective.
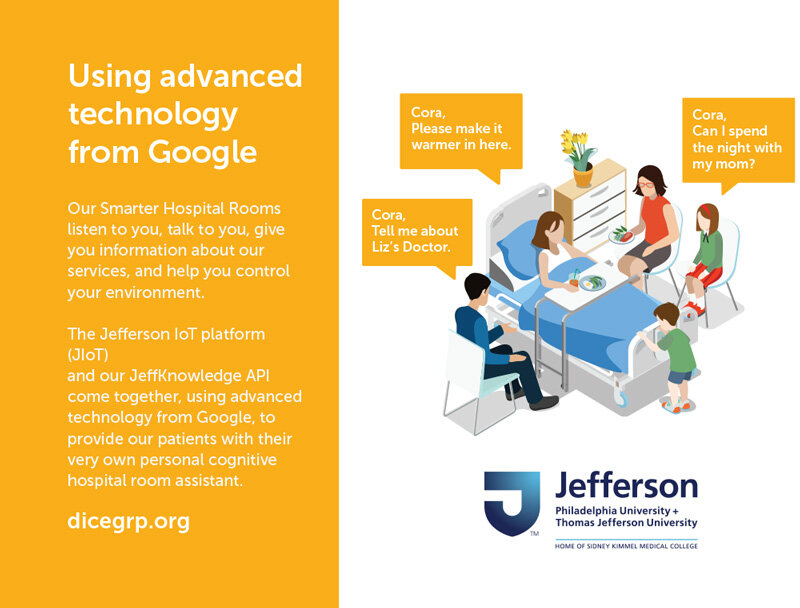
Promotional Material
Our team distributed this palm card I designed at HIMSS 2018, Google booth.
Getting starting
Having no prior experience with voice design, I …
Read several VUI books about best practices to understand the benefits and limitations of voice interface (distinguishing conversational voice interface from direct speech-to-text/command-based voice interaction.) (recommended reading list at that time)
Embraced surrogacy learning: I interviewed pioneers including Google Voice Interface researchers.
Became familiar with existing platforms including usage statistics and critiques of each major platform. Check out this one on accents from 2017.
Next, I began primary research phase:
Gather sample of patient insights:
surprisingly the voice of patient had been assumed prior to my arrival. I worked directly with our clinical fellow to design a patient feedback methodology.
We met with a small sample of patients to review a series of questions in a simple survey we created. These insights were powerful and helped orient the focus of our feature recommendations. We also better understood how a product like this would be perceived and started to consider what tools and approaches would be needed to introduce patients to this often uncommon interaction with this emerging technology.Synthesize findings and translate interview material into to focused feature recommendations.
Among key constraints: Balancing feasibility of the medium with patient requests.
For example: tell me about my medical condition and what medicines I should take were out of scope for early versions of a product like this.
We wanted to pair common questions that were relevant to healthcare environment yet feasible to respond to. For example - explaining procedures or patient condition was not going to be a simple feature to design and build.
Among my early recommendations: use Alexa or Google Home as base platform and layer on hospital specific info such as ordering from cafeteria, visiting hours, room calling, communicating with nurse’s station without needing to find call-bell button.
In 2017, cloud-based servers that offered HIPAA compliance certification were difficult to identify and slowed the pace of implementation. This presenting important design constraints when crafting skills patients would find valuable. One of the skill sets we recommended was control of TV in hospital room - thus saving patients hassle searching for remotes.
For future consideration, we noted great potential for smart speaker devices to:
Serve as communication mechanism between nursing staff and patient (in effort to reduce dependency on tethered call bell)
Order meals and checking meal order status - having potential to save hospitals money and improve patient satisfaction. One particular use case, that impacts patient experience: new patient arrivals may miss meal collection and be satisfied with default meal provided. Building a simple skill would require tremendous interoperability effort and we didn’t have sufficient data to correlate this feature to patient satisfaction to support the investment of resources.
Phase 2: Package Findings, design skills and intents
Collaborate with clinical fellow to generate demographics profiles of each pilot site candidate.
Working with development teams, understand tech stack capabilities
Coalesce stakeholder and patient feedback (#2) into key feature requests
Plot feature requests along priority matrix
Map feature requests with HIPPA compliance feasibly
Indexing key features and transitioning them into catalogue of skills and intent patients can speak after activating wake word.
Expand catalogue into subset of alternatives (many ways to ask the same question)
Phase 3: Start planning Pilot
Revisit demographics of clinical units with project manager and nursing managers for potential pilot sites - project dates
Generated validation checklist with Clinical Fellow (for QA testing before deployment)
Design prototype of brief patient-facing booklet for the pilot - to introduce patient to this new technology and convey features and limitations. This booklet doubled as a mechanism to collect feedback from patients. It included example utterances for patients to try.
During this phase, I worked with senior leadership to identify talented UX researcher to shepard this project further and I transitioned out of the project. prioritize and test feature requests. This system was able to scale and be compatible with scrum team’s development cycles.
To help senior leadership cast the vision and keep momentum going for this project, I spent time crafting a vision deck. I’m very proud of the copy I wrote for this deck.
Our team presented this deck at a Google both in 2017 and slides from this deck appeared in a keynote delivered by our president and CEO and Adobe Max address in 2018.
Whenever this smart speaker project is showcased to a group of healthcare providers there is a wealth of creative ideas sparked and brainstorming session quickly begins.
Conclusion
Over the past three years, this concept of placing smart speakers in hospital rooms has started to take hold around the country. My early assertions were that the product stack should be built on top of Alexa skills or Google voice platform. In early 2019, Cedar Sinai announced they had partnered with Alexa to do just that and deploy a small pilot. To date, I’ve not see results published from this study but believe they will be instrumental to healthcare systems considering leveraging this platform for patient and provider benefit.
Here is a recent summary of this initiative posted on DICE Group blog.